Why do antiviral drugs often have side effects in host cells? Antiviral drugs often have side effects in host cells because they target both the virus and the host cells, which can cause unintended consequences. Antiviral drugs are designed to inhibit the replication and spread of a virus within the body.
These drugs work by targeting specific viral proteins or enzymes, disrupting their functions, and preventing the virus from replicating. However, since viruses rely on host cells for their survival and replication, antiviral drugs also interact with the host cells. This interaction can lead to side effects, as the drugs may interfere with normal cellular processes or damage healthy cells.
Additionally, the specific mechanisms of action of different antiviral drugs and their impact on host cells vary, leading to a range of possible side effects. Understanding the unique chemistry between drugs, viruses, and host cells is essential for developing more effective and safe antiviral treatments.
Understanding The Mechanisms Behind Antiviral Drug Side Effects
Antiviral drugs often have side effects on host cells due to the complexity of their interactions. These medications are designed to target specific viral replication processes within the infected cells. However, they can also impact healthy cells in the body, leading to side effects. The mechanisms behind these interactions involve the drug’s mode of action, which may interfere with cellular processes necessary for both viral replication and normal cell functioning. Additionally, the structure and function of host cell components may influence the drug’s effectiveness, leading to unintended consequences. Careful study and research are necessary to better understand these mechanisms and develop more targeted antiviral therapies with reduced side effects. By gaining a deeper understanding of the intricacies of antiviral drug interactions with host cells, scientists can strive for more effective and safer treatment options.
Unravelling The Why: Factors Influencing Side Effects In Host Cells
Antiviral drugs, while effective in combating viral infections, often come with side effects in host cells. Understanding the underlying factors that contribute to these side effects is crucial to developing safer and more targeted treatment options. One key factor is the drug’s specificity in interacting with host cells. Different antiviral drugs have varying degrees of specificity, with some targeting specific viral enzymes or proteins. The interaction between the drug and host cell factors also plays a significant role. Certain host cell factors can enhance or diminish the drug’s effectiveness, leading to side effects. Genetic variations in host cells can make individuals more susceptible to these side effects. Individuals with specific genetic variations may metabolise or respond to drugs differently, increasing the likelihood of adverse reactions. By unravelling the reasons behind antiviral drug side effects in host cells, researchers can develop strategies to minimise or eliminate these detrimental effects and improve patient outcomes.
Balancing Act: Minimising Side Effects While Maximising Efficacy
Antiviral drugs are crucial in treating viral infections, but they often come with side effects in host cells. This occurs because these medications must strike a delicate balance between minimising side effects and maximising efficacy. To achieve this, various strategies can be employed.
Optimising Drug Delivery to Minimise Host Cell Damage: Scientists focus on developing drug delivery methods that specifically target viral components while minimising interaction with healthy cells. This can reduce the potential for adverse effects.
Monitoring and Management of Antiviral Drug Side Effects: Regular monitoring of patients receiving antiviral treatment helps identify and manage any potential side effects promptly. Adjustments can be made to the dosage or the medication itself to mitigate adverse reactions.
By implementing such strategies, healthcare professionals aim to enhance the efficacy of antiviral drugs while minimising their impact on host cells.
Host Cells of Viruses: Understanding the Intricate Relationship
Viruses are fascinating microorganisms that exist on the border between living and non-living entities. Unlike bacteria, fungi, or other organisms, viruses cannot carry out metabolic processes or replicate on their own. Instead, they rely on host cells to carry out their life cycle. In this blog post, we will delve into the intriguing world of host cells for viruses and explore how viruses interact with their hosts.
The Diverse World of Viruses
Viruses are incredibly diverse in terms of size, structure, and genetic material. Some viruses, like the influenza virus, have a single-stranded RNA genome, while others, like the herpesvirus, have a double-stranded DNA genome. These viruses infect a wide range of hosts, including humans, animals, plants, and even bacteria. To infect these hosts, viruses must first gain entry into a suitable host cell.
Host Cells: The Virus’ Home Away from Home
A host cell is a living organism that a virus infects and uses for its replication and survival. Each virus has a specific host range, meaning it can only infect certain types of cells or organisms. The interaction between viral surface proteins and host cell receptors determines this specificity. When a virus encounters a compatible host cell, it initiates a series of events that ultimately lead to the infection process.
The Infection Process
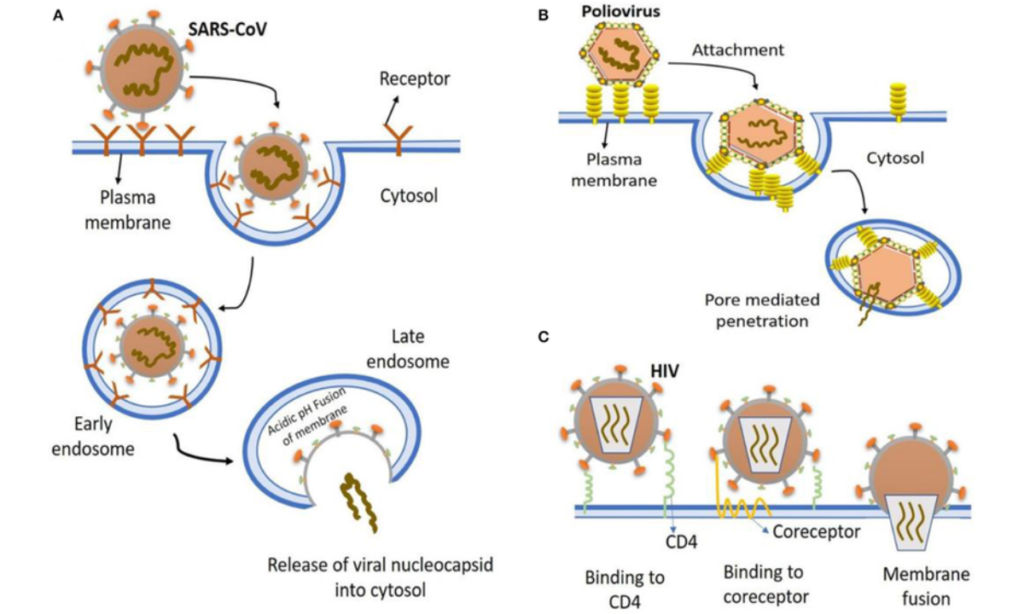
- Attachment: The first step in the infection process is attachment. Viruses have surface proteins or spikes that bind to specific receptors on the host cell’s surface. This binding is particular, like an essential fitting into a lock. Once attached, the virus gains entry into the host cell.
- Entry: After attachment, the virus must enter the host cell. The methods of entry vary among different viruses. Some viruses enter the host cell by fusing directly with the cell membrane, while others enter the cell through a process known as endocytosis.
- Replication and Transcription: Once inside the host cell, the virus takes control of the cellular machinery to replicate its genetic material and produce new viral particles. DNA viruses use the host cell’s machinery to transcribe their DNA into RNA, while RNA viruses directly use the host’s ribosomes to make viral proteins.
- Assembly: The newly synthesised viral components are assembled into new virus particles within the host cell.
- Release: Finally, the newly formed viruses are released from the host cell. This can occur through cell lysis (the cell bursts open), or in some cases, viruses are released more subtly without killing the host cell.
Examples of Host Cells for Viruses
- Human Host Cells: Numerous viruses, such as the human immunodeficiency virus (HIV), infect human host cells, targeting specific cell types like T cells, macrophages, or epithelial cells.
- Animal Host Cells: Viruses also infect animals and can target a wide range of tissues, including the respiratory tract, digestive system, and nervous system.
- Plant Host Cells: Plant viruses infect various plant cells, leading to diseases that impact agriculture.
- Bacterial Host Cells: Bacteriophages are viruses that infect and replicate within bacterial cells, often leading to the destruction of the host bacterium.
Viruses are masterful manipulators of host cells, hijacking their machinery to reproduce and spread. Understanding the intricacies of host-virus interactions is crucial for developing antiviral therapies and vaccines. As science continues to advance, our knowledge of the host cells of viruses grows, providing hope for more effective treatments and a deeper understanding of the delicate balance between viruses and their hosts.
Which of the Following Leads to the Destruction of Host Cells?
The human body is a complex ecosystem of cells, each with a specific function and role to play in maintaining our overall health. However, this intricate balance can be disrupted when external factors or pathogens invade our system. One of the critical mechanisms employed by the immune system to combat such intruders is the destruction of host cells that have been compromised. In this blog, we will explore the various factors and processes that can lead to the destruction of host cells.
Viral Infections:
Viruses are microscopic infectious agents that can only reproduce within the living cells of an organism. When a virus infects a host cell, it takes over the cell’s machinery to replicate itself. This often leads to the host cell’s destruction, as the newly formed viruses burst out, causing cell lysis or cell death.
Immune Response:
The immune system plays a crucial role in defending the body against infections. Immune cells such as cytotoxic T cells and natural killer (NK) cells can recognize infected or abnormal host cells. These immune cells can release toxic substances, like perforin and granzymes, which puncture holes in the infected cells’ membranes, causing them to die.
Apoptosis:
Apoptosis, often referred to as programmed cell death, is a highly regulated process that eliminates damaged, infected, or unnecessary cells. It is a fundamental mechanism for maintaining tissue homeostasis and plays a significant role in removing host cells that pathogens or other factors have compromised.
Bacterial Infections:
While bacteria primarily reproduce outside host cells, some bacterial species can invade host cells. In some cases, the host cell may respond by initiating apoptosis to limit the infection. Additionally, the immune system can also target infected host cells, leading to their destruction.
Toxic Chemicals and Substances:
Exposure to toxic chemicals or substances can also lead to the destruction of host cells. These poisonous agents can disrupt the cell membrane, interfere with essential cellular processes, or trigger apoptosis. Examples include exposure to certain drugs, environmental toxins, or harmful molecules produced by bacteria.
Autoimmune Disorders:
In some autoimmune diseases, the immune system mistakenly targets and attacks healthy host cells and tissues. This can lead to the destruction of these cells and tissues, causing various health problems. Examples of autoimmune disorders include rheumatoid arthritis, multiple sclerosis, and type 1 diabetes.
Radiation and Cancer Therapy:
Radiation therapy and specific cancer treatments, such as chemotherapy, are designed to kill rapidly dividing cells, which include both cancerous and healthy cells. Unfortunately, this can result in the destruction of host cells in the process of treating cancer.
The destruction of host cells can occur due to various factors and processes, ranging from viral infections and immune responses to toxic chemicals and autoimmune disorders. While these mechanisms are essential for maintaining our health and defending against threats, they can sometimes lead to collateral damage. Understanding how and why host cells are destroyed is critical in the fields of medicine, immunology, and microbiology, as it informs our efforts to combat infections and develop treatments for various diseases.
Frequently Asked Questions: Why Do Antiviral Drugs Often Have Side Effects in Host Cells?
Why do viruses depend on host cells?
Viruses depend on host cells because they require the cell’s machinery to reproduce.
What Viral Structure Allows Viruses to Attach to a Host Cell?
The viral structure that allows viruses to attach to a host cell is called a viral receptor.
What feature of the viral life cycle makes it difficult to produce antiviral drugs?
The problematic feature of the viral life cycle to target with antiviral drugs is ________.
How do viruses interact with cells?
Viruses interact with cells by attaching to receptors on the cell surface and penetrating the cell membrane.
Conclusion
Antiviral drugs play a crucial role in treating viral infections by targeting specific viral components and inhibiting their replication. However, due to the similarities between host cells and viral cells, these drugs can also affect normal cellular functions. This leads to the occurrence of side effects in host cells.
The complex nature of viruses makes it challenging to develop antiviral drugs that solely target viral components without affecting host cells. Scientists continue to conduct extensive research to uncover new antiviral drug targets and develop strategies that minimise side effects in host cells.
Understanding the mechanisms behind antiviral drug side effects in host cells is essential for improving drug development and enhancing patient safety. By gaining insights into how antiviral drugs interact with host cells, scientists can improve drug design and minimise adverse effects on vital cellular functions.
In the future, advancements in technology and research may lead to the development of antiviral drugs with minimal side effects in host cells, improving treatment options for viral infections, and ultimately benefiting human health.

